Outcomes
 Basic research
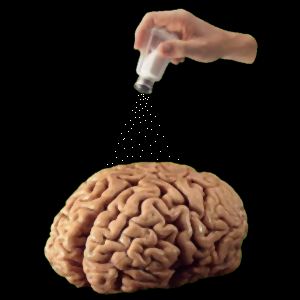
with clinical relevance. The objective of our
research program is to
define the neurobiology of hypothalamic circuits that mediate fluid
homeostasis. While we focus on fundamental
issues related to these networks at the molecular, cellular and systems
level, many of our studies are currently performed in the context of
important clinical problems including:
Basic research
with clinical relevance. The objective of our
research program is to
define the neurobiology of hypothalamic circuits that mediate fluid
homeostasis. While we focus on fundamental
issues related to these networks at the molecular, cellular and systems
level, many of our studies are currently performed in the context of
important clinical problems including:
- Salt-dependent hypertension
- Osmoregulatory dysfunction during septic shock
- Dehydration
- Hyponatremia
Physiology comes first. From a trainee's perspective, studying mechanisms that underlie normal brain function (rather than being constrained to a disease model) provides an opportunity to learn fundamental principles and advanced experimental techniques that are broadly applicable to other models or systems. This approach has allowed trainees to pursue careers in various aspects of the life sciences (see alumni). Current trainees are currently exploring questions such as:
- How do neurons detect changes in core body temperature?
- How do central clock neurons regulate specific neuroendocrine rhythms?
- How do astrocytes detect changes in fluid osmolality?
- How is burst firing modulated by afferent inputs?
The new knowledge created by addressing such questions is then used to explore how disease (e.g. septicemia), genetic mutations (spontaneous or inherited), behavior (e.g. excessive salt intake) and environmental factors (changes in ambient heat) can cause osmoregulatory deficits.
What other clinical conditions are targeted by this research? Defining the mechanisms by which neurons wired within osmoregulatory circuits detect changes in core body temperature, blood sodium concentration and plasma osmolality could shed light on how environmental factors such as salt intake, heat exposure, shift work, jet-lag and exercise normally cause adaptive changes in fluid-electrolyte balance to maintain hydration and blood pressure. Pathological changes in these mechanisms have been linked to:
- hyponatremia and edema following myocardial infartion
- hyponatremia caused by drugs (e.g. ecstasy)
- hyponatremia during hyperglycemia linked to diabetes mellitus
- hyponatremia during liver disease
- increased risk of dehydration in elderly
- Edema during pregnancy
- circadian (night time) polyuria/enuresis
- neurogenic diabetes insipidus
- syndrome of inappropriate vasopressin release (SIADH)
- hypernatremia during septic shock
- hypernatremia caused by ethanol
- Salt-dependent hypertension
- Osmoregulatory dysfunction during septic shock
- Dehydration
- Hyponatremia
Physiology comes first. From a trainee's perspective, studying mechanisms that underlie normal brain function (rather than being constrained to a disease model) provides an opportunity to learn fundamental principles and advanced experimental techniques that are broadly applicable to other models or systems. This approach has allowed trainees to pursue careers in various aspects of the life sciences (see alumni). Current trainees are currently exploring questions such as:
- How do neurons detect changes in core body temperature?
- How do central clock neurons regulate specific neuroendocrine rhythms?
- How do astrocytes detect changes in fluid osmolality?
- How is burst firing modulated by afferent inputs?
The new knowledge created by addressing such questions is then used to explore how disease (e.g. septicemia), genetic mutations (spontaneous or inherited), behavior (e.g. excessive salt intake) and environmental factors (changes in ambient heat) can cause osmoregulatory deficits.
What other clinical conditions are targeted by this research? Defining the mechanisms by which neurons wired within osmoregulatory circuits detect changes in core body temperature, blood sodium concentration and plasma osmolality could shed light on how environmental factors such as salt intake, heat exposure, shift work, jet-lag and exercise normally cause adaptive changes in fluid-electrolyte balance to maintain hydration and blood pressure. Pathological changes in these mechanisms have been linked to:
- hyponatremia and edema following myocardial infartion
- hyponatremia caused by drugs (e.g. ecstasy)
- hyponatremia during hyperglycemia linked to diabetes mellitus
- hyponatremia during liver disease
- increased risk of dehydration in elderly
- Edema during pregnancy
- circadian (night time) polyuria/enuresis
- neurogenic diabetes insipidus
- syndrome of inappropriate vasopressin release (SIADH)
- hypernatremia during septic shock
- hypernatremia caused by ethanol